Understanding the Risks of Hysterectomy: An Expert Guide by Leading Obstetricians & Gynecologists
In the realm of women’s health, hysterectomy remains one of the most common and significant surgical procedures performed worldwide. As an essential intervention for various gynecological conditions, it can offer relief from chronic pain, heavy bleeding, and other health issues. However, like all surgeries, hysterectomy carries inherent risks that women must understand thoroughly before making informed decisions. This comprehensive guide, crafted by leading doctors in obstetrics & gynecology at drseckin.com, aims to shed light on the risks of hysterectomy, encompassing immediate, short-term, and long-term considerations, thus empowering women with knowledge and confidence regarding their health options.
What is a Hysterectomy and Why It Is Performed
A hysterectomy involves the surgical removal of the uterus, with or without the removal of surrounding tissues such as the cervix, fallopian tubes, and ovaries. This procedure is typically recommended for conditions including uterine fibroids, prolapse, endometriosis, abnormal bleeding, and sometimes for cancer treatment. Despite its proven effectiveness, understanding the associated risks of hysterectomy is crucial for women contemplating this intervention.
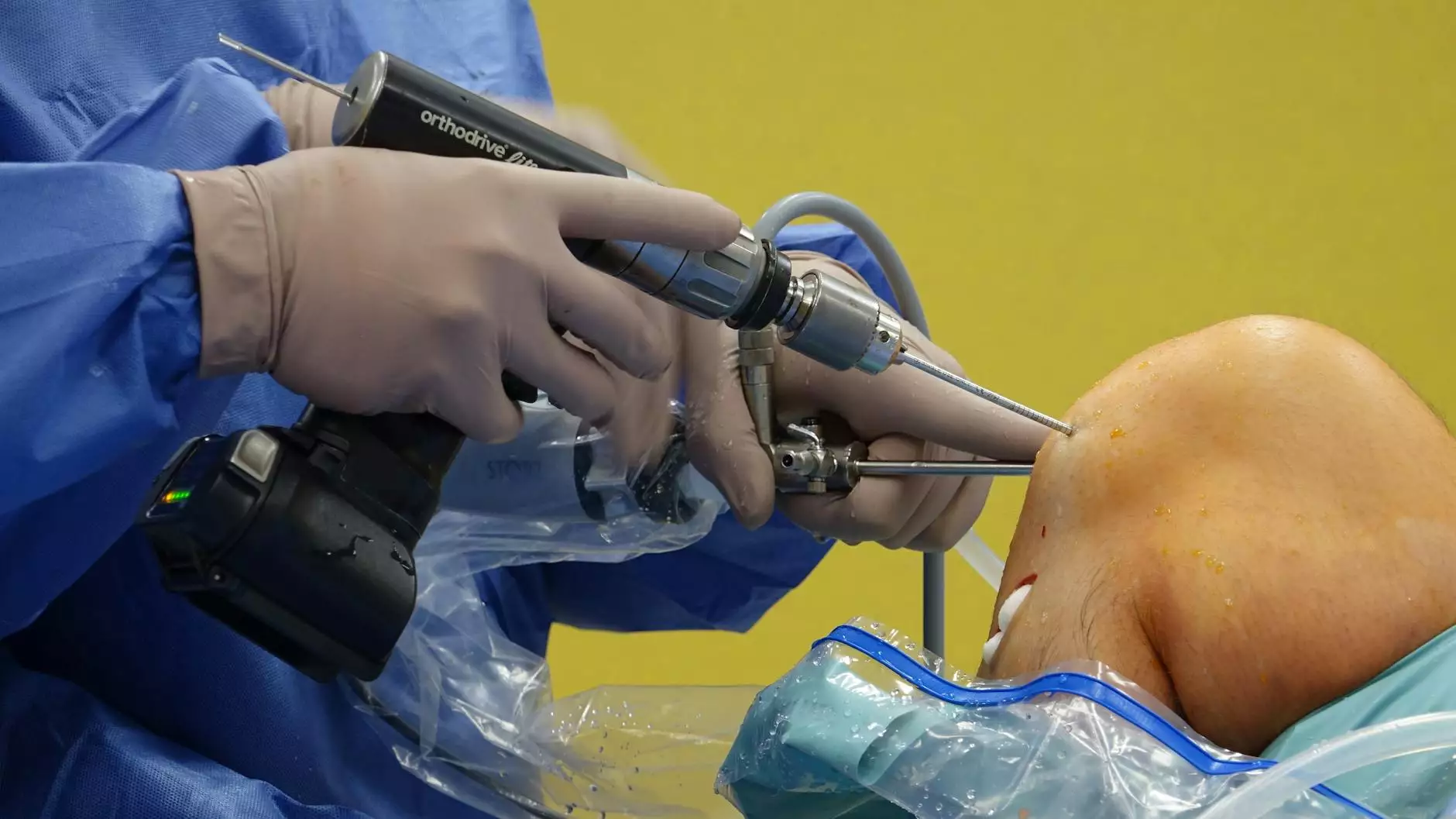
Types of Hysterectomy and Their Implications for Risk
Subtotal (Partial) Hysterectomy
Removes the uterus while leaving the cervix intact. This procedure may carry a lower risk of certain complications but still involves significant considerations.
Total Hysterectomy
Removes the entire uterus and cervix. It is the most common type and has specific risks associated with removal of reproductive organs.
Radical Hysterectomy
A more extensive removal involving surrounding tissues, often performed for cancer treatments. The risk profile increases correspondingly.
Immediate and Short-Term Risks of Hysterectomy
While hysterectomy is generally safe when performed by experienced obstetricians & gynecologists, it still carries immediate and short-term risks that could impact recovery and overall health:
- Bleeding: Excessive intraoperative or postoperative bleeding might necessitate blood transfusions.
- Infection: Surgical site or pelvic infections are potential complications.
- Organ Injury: Accidental damage to surrounding organs, such as the bladder or intestines.
- Adverse Reactions to Anesthesia: Anesthetic complications can include allergic reactions or respiratory issues.
- Blood Clots: Deep vein thrombosis (DVT) or pulmonary embolism (PE) risk increases post-surgery.
Understanding the Risks of Hysterectomy: Long-Term and Psychological Effects
Beyond the immediate surgical risks, women should be aware of the long-term impacts and psychological considerations associated with hysterectomy:
Hormonal Imbalances and Ovarian Function
In cases where the ovaries are removed (oophorectomy), women may experience early menopause symptoms such as hot flashes, mood swings, decreased libido, osteoporosis, and increased cardiovascular risk. Even when ovaries are preserved, some deterioration in hormonal function may occur over time.
Impact on Sexual Function
Some women report changes in sexual desire, sensation, or comfort following hysterectomy. However, outcomes vary based on the type of hysterectomy performed and individual health factors.
Psychological and Emotional Considerations
The removal of reproductive organs can lead to feelings of loss or grief for some women, especially if the procedure addresses cancer or fertility issues. Counseling and psychological support are often recommended to navigate these emotional responses effectively.
Potential for Pelvic Floor Disorders
Hysterectomy may alter pelvic support structures, sometimes leading to urinary incontinence or pelvic organ prolapse, which could necessitate additional treatment.
Specific Risks of Hysterectomy Related to Age and Medical Conditions
The patient's age and overall health significantly influence the risk profile:
- Older women face increased surgical risks due to comorbid conditions such as hypertension, diabetes, or cardiovascular disease.
- Women with obesity have higher risks of complications including wound healing issues and infections.
- Patients with prior abdominal surgeries may encounter adhesions, increasing surgical complexity and risk.
Alternatives to Hysterectomy: Non-Surgical Options and Their Risks
Before opting for hysterectomy, exploring alternative treatments is essential, especially considering the risks of hysterectomy. Non-invasive or minimally invasive options can be effective for certain conditions:
- Myomectomy: Removal of fibroids while preserving the uterus.
- Uterine artery embolization: Cutting off blood supply to fibroids to shrink them.
- Hormonal therapies: Using medications to manage bleeding or pain.
- Endometrial ablation: Destroying the uterine lining to reduce bleeding.
While these alternatives may have fewer risks, they are not suitable for all cases. Consulting with an experienced doctor in obstetrics & gynecology is essential to determine the most appropriate course of action based on individual health status and condition severity.
Preoperative Preparation and Risk Minimization Strategies
Proper planning can significantly reduce the risks of hysterectomy. Recommended strategies include:
- Comprehensive preoperative evaluation, including imaging and lab tests.
- Addressing any existing infections or health issues prior to surgery.
- Ensuring optimal blood pressure, glucose control, and overall health optimization.
- Discussing anesthesia risks and postoperative care plans with your surgical team.
- Choosing an experienced surgical team skilled in minimally invasive techniques where appropriate.
Postoperative Care and Long-Term Health Monitoring
Follow-up and ongoing health management are vital components of recovery and long-term wellbeing:
- Monitoring for signs of infection, bleeding, or other complications.
- Gradual return to activity, with guidance from your healthcare provider.
- Addressing emotional and psychological needs, including counseling if necessary.
- Maintaining bone health with adequate calcium and vitamin D intake, especially after ovarian removal.
- Regular gynecological check-ups to monitor overall reproductive and pelvic health.
Empowering Women with Knowledge About the Risks of Hysterectomy
It is essential for women to be fully informed about the risks of hysterectomy to make empowered, thoughtful health decisions. Consulting with qualified, experienced doctors in obstetrics & gynecology at reputable clinics such as drseckin.com provides access to expert guidance tailored to individual needs.
In conclusion, while hysterectomy can be a life-changing and beneficial procedure for many women, understanding its potential risks—both immediate and long-term—is crucial. With comprehensive medical advice, advanced surgical techniques, and supportive postoperative care, women can navigate their health journeys with confidence and peace of mind.
Seek Expert Care for Safe and Informed Treatment Decisions
If you are considering a hysterectomy or want to know more about your gynecological health options, consulting with specialized obstetricians & gynecologists at a trusted healthcare provider ensures you receive personalized, safe, and effective care. Prioritize your health, and make informed choices today for a healthier tomorrow.









